by Danielle Dunn
'Refractory', 'intractable' and 'drug resistant' are all terms for epilepsy which does not respond readily to antiepileptic medication.
The world's leading epilepsy body, the International League Against Epilepsy (ILAE), prefers to use the term 'drug resistant epilepsy' and defines this as:
The failure of adequate trials of two tolerated and appropriately chosen and used AED schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom.
Check out the ILAE consensus document here:
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1528-1167.2009.02397.x
As an epileptic patient it is really important to identify if you are entering a situation of drug resistant epilepsy early in the course of management as this is a pivotal point as to what treatment is most likely to help. Being on the most effective management plan for your type of epilepsy gives you the greatest chance of timely seizure control and a better overall quality of life.
So, let’s unpack the definition statement above to work out what exactly is drug resistant epilepsy.
The overall theme of the statement describes drug resistant epilepsy as being seizures that do not come under control promptly with antiepileptic medication. The ILAE makes this more precise by defining the number of drug trials used before labelling the epilepsy as drug resistant. There is good reason why they state the use of two drug trials.
Different studies from around the world and over time looking at the response rate of patients to antiepileptic medication trials come to the same conclusions. Around 50% of epileptic patients will gain seizure control with the first antiepileptic medication trial and another 15-20% will gain control with the second medication they trial. Once you get to the point where the first two antiepileptic medications have failed to control the seizures, the likelihood of the third antiepileptic medication trial to control the seizures drops down to just 1-3%. If medications are combined the seizure control rate increases slightly to 3-5%. That leaves around a third of epileptic patients who do not gain seizure control with antiepileptic medication. The pie chart below illustrates this information from a study following 525 peoples epilepsy journey's as they were first diagnosed and treated for epilepsy.
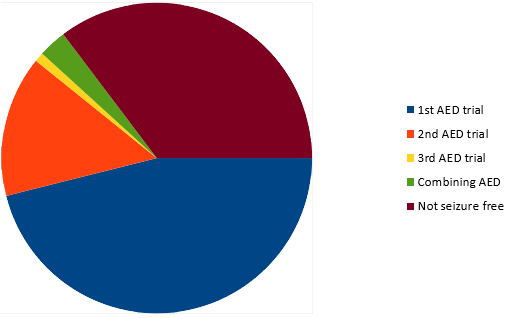
Seizure free rates with different strategies
Kwan P, Brodie MJ. (2000). Early identification of refractory epilepsy. N Eng J Med. 2000 Feb 3;342(5):314-9.
The drug resistant epilepsy definition is further refined by specifying that the trials are:
- adequate (sufficient dose and period of time trialled)
- tolerated (minimal side effects)
- appropriately chosen (for the patient’s epilepsy and seizure type)
The final part of the definition requires that the seizure freedom is sustained which is defined as the interval between seizures being at least 12 months.
Despite the huge addition of antiepileptic medications being made available over the last few decades, there has been very little change to the pie chart above. Around a third of patients with epilepsy still do not gain seizure freedom with antiepileptic medications even if they trial the newest drugs on the market.
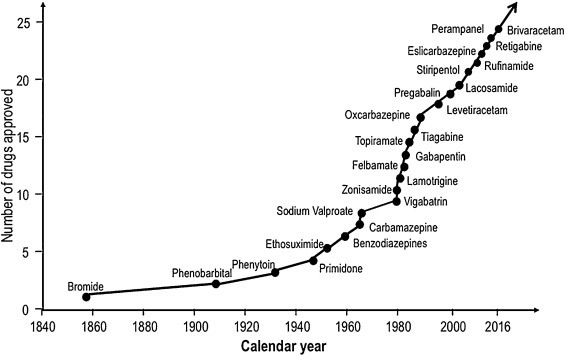
New Antiepileptic Drugs Approved for use over Time
P. Kwan. Refractory epilepsy: natural history and pathogenesis. PhD thesis
Department of Medicine and Therapeutics, University of Glasgow, Glasgow, UK (2000)
The tipping point...
To advocate for the best epilepsy management plan for your child or yourself it is crucial you know what part of the pie chart you fall in. Ideally your neurologist should keep you fully informed as to the likelihood of each management option they offer you to produce good seizure control. If you have had two or more adequate, tolerated and appropriately chosen antiepileptic drug trials and still do not experience sustained seizure freedom then the next best step is a Ketogenic Diet trial.
The success rate of Ketogenic Dietary Therapy in achieving a maximal and rapid reduction in seizures outweighs that of further drug trials in the case of drug resistant epilepsy. Ketogenic Therapy also has the additional benefits of often improving cognition and mood and sometimes allowing for a reduction in the dose of concurrent antiepileptic medications. For this reason, a 3-6 month ketogenic diet trial supervised by a Specialised Ketogenic Registered Dietitian and Neurologist should be initiated at the point of first diagnosing drug resistant epilepsy.
As the seizure free rates of sequential antiepileptic medication trials is predictable, the response rate to a Ketogenic Diet trial is also predictable. Research throughout the last century in different clinics around the world has found similar results. Around 50% of patients have their seizures reduced by at least half with a ketogenic diet trial, 30% of which gain 90% control of their seizures and 10-15% become seizure free. What is not currently predictable is what category you will fall into when trialling antiepileptic medications or a Ketogenic Diet, hence the trial and error process. Maybe with time there will be more precision in choosing the best management regime for the individual patient.
Poorly controlled seizures take their toll on the entire family and lead to diminished health, educational and social outcomes. To live well with Epilepsy it is paramount that seizures are minimised as quickly as possible through appropriate and effective management regimes. By being fully informed as a patient or caregiver you are empowered to advocate for the best treatment plan for your situation.